Disclaimer [ENGLISH]
Definition
A bacterial infection of the middle ear (the space behind the eardrum)
Health Information
Symptoms
-
Pain.The most common symptom of an ear infection is pain.
- Older children can tell you that their ears hurt.
- Younger children may only seem irritable and cry.
- You may notice this more during feedings because sucking and swallowing may cause painful pressure changes in the middle ear.
- This usually starts after having cold symptoms for a few days – like stuffy nose, runny nose and cough.
- Decreased appetite.
- Trouble sleeping.
- Fever. Your child’s temperature might be normal or could be elevated, even as high as 104°F.
-
Ear drainage.
- A small number of children develop a tear (or rupture) of the eardrum because of pressure in the middle ear.
- You might notice yellow or white fluid, possibly blood-tinged, draining from your child’s ear. It might smell bad. The fluid will look different from normal earwax (which is orange-yellow or reddish-brown).
- Pain and pressure often decrease after this drainage begins, but this doesn’t always mean that the infection is going away. If this happens it’s not an emergency, but your child will need to see their pediatrician.
-
Trouble hearing.
- Your child might have trouble hearing for several weeks.
- This is usually temporary and clears up after the fluid from the middle ear drains away.
There are many other reasons why your child’s ears hurt besides an ear infection.
An ear infection cannot be diagnosed over the phone or during a video visit; your child’s eardrum must be examined to confirm fluid buildup and signs of inflammation.
Diagnosis
A middle ear infection is diagnosed by looking at the eardrum. It will be bulging and have pus behind it.
Cause
-
How do ear infections develop?
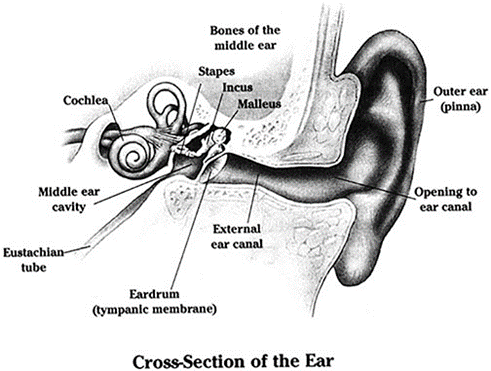
- The ear has 3 parts—the outer ear, middle ear, and inner ear.
- A narrow channel (eustachian tube) connects the middle ear to the back of the nose.
- Mucus and fluid can enter this tube causing a buildup of fluid in the middle ear when a child has a cold or allergies.
- If bacteria or a virus infects this fluid, it can cause swelling and pain in the ear.
- Ear infections are the most common bacterial infection in young children, between the ages of 6 months and 3 years of age and are a common problem until age 8.
- 90% of children have at least 1 ear infection. Frequent ear infections occur in 20% of children.
- Ear infections cannot be spread to others.
Care Advice
-
Overview:
- Most ear infections are not cured after the first dose of antibiotic.
- Most children get better slowly over 2 to 3 days.
-
Antibiotic by Mouth:
- Not all bacterial ear infections require antibiotics. Some may be observed without antibiotics. Many times, pain and fever improve in 1-2 days without an antibiotic.
- Your child’s healthcare provider might give you a prescription and tell you to start it in a few days if symptoms are not improving.
- Your child’s healthcare provider might decide to treat with antibiotics right away.
- If prescribed, antibiotics kill the bacteria that are causing the ear infection. Give the antibiotic as directed by your child’s healthcare provider and do not stop the antibiotic earlier than instructed, even if your child’s symptoms seem improved.
-
Fever & Pain:
- For fevers above 102° F (39° C) or for pain, give acetaminophen (such as Tylenol) or ibuprofen (such as Motrin or Advil). See Ibuprofen dosage table and Tylenol dosage table.
- For ALL fevers: Keep your child well hydrated. Give lots of cold fluids.
- Put a cold wet washcloth on the outer ear for no more than 20 minutes. This should help the pain until the pain medicine starts to work.
- Some children prefer a heating pad or heat pack instead.
-
Eardrops:
- If pain medicine does not help the pain, you can try eardrops of plain olive oil or mineral oil. Use 3 drops every 4 hours as needed.
- Don’t use these kinds of eardrops if your child has ear tubes or if your child has a hole in the eardrum.
-
Limits:
- Swimming is fine as long as there is no drainage from the ear and your healthcare provider has not diagnosed a tear in the eardrum.
- Air Travel
- Children with ear infections can travel safely by aircraft if they are taking antibiotics. For most, flying will not make their ear pain worse.
- During descent (coming down for landing) have your child swallow fluids. Sucking on a pacifier may help as well. Children over age 6 can chew gum.
-
Ear Discharge:
- If pus or blood is draining from the ear, the eardrum probably has a small tear. Discharge can also occur if your child has ear tubes.
- Most often, this heals in 2 to 3 days.
- Wipe the discharge away as you see it.
- Do not plug the ear canal with cotton.
-
What to Expect:
- If your child is prescribed antibiotics, they should be getting better after 2 or 3 days of treatment.
- The fever should be gone by 2 days (48 hours).
- The ear pain should be better by 2 days. It should be gone by 3 days (72 hours).
-
Return to School:
- Your child can go back to school when any fever is gone
- Your child should feel well enough to join in normal activities.
-
Ear re-check:
- In certain situations, your healthcare provider might request a follow-up in 2 to 3 weeks. At that visit, the eardrum will be checked to make sure that the infection is cleared up and no more treatment is needed.
- Your healthcare provider might also want to test your child's hearing.
- Follow-up exams are very important, particularly if the infection has caused a hole in the eardrum.
Call Your Doctor If:
- Fever lasts more than 2 days after starting antibiotics.
- Ear pain lasts more than 3 days after starting antibiotics.
- Ear discharge is not better after 3 days after starting antibiotics.
- Your child develops new or worsening symptoms, or you think your child needs to be seen.
Recurrent Ear Infections
- Prevention of recurrent ear infections
- Avoid exposure to tobacco smoke.
- Breastfeeding may decrease the risk of frequent colds and ear infections.
- Avoid bottle propping. Hold your baby with their head higher than their stomach.
- If your child is older than 1 year, throw away pacifiers or limit to daytime use
- During the first year of life, try to reduce contact with other sick children.
- Get all recommended vaccines.
- Control any allergies your child might have. Monitor for snoring and discuss this with your child’s healthcare provider.
- Does my child need ear tubes?
- Ear tubes are also called PE tubes, tympanostomy tubes, and ventilation tubes.
- They are tiny plastic tubes that are placed across the eardrum by an ear surgeon (ENT or otolaryngologist)
- Reasons your child might need ear tube surgery:
- Fluid has been present in the middle ear for over 3 months. Both ears have fluid.
- Hearing loss.
- More than 3 ear infections in 6 months.
- More than 4 ear infections in 12 months.
- Ear infections that do not clear up after trying many antibiotics.
This publication was adapted from information within American Academy of Pediatrics Patient Education Handouts
Reviewed by: AR D.O. | 06/2023


